Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
COPD (Chronic Obstructive Pulmonary Disease)
Condition Basics
What is chronic obstructive pulmonary disease (COPD)?
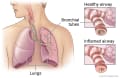
COPD (chronic obstructive pulmonary disease) is a lung disease that makes it hard to breathe because air doesn't flow easily in and out of your lungs.
Chronic bronchitis and emphysema are two lung problems that are types of COPD.
- Chronic bronchitis. When you have chronic bronchitis, the airways that carry air to the lungs (bronchial tubes) get inflamed and make a lot of mucus. This can narrow or block the airways, making it hard for you to breathe. It can also make you cough.
- Emphysema. With this disease, the tiny air sacs in the lungs are damaged and lose their stretch. Less air gets in and out of the lungs, which makes you feel short of breath.
COPD often gets worse over time. You can't undo the damage to your lungs. But you can take steps to help prevent more damage and to feel better.
What causes it?
COPD is often caused by smoking. Air pollution also causes COPD. Other things that may lead to COPD include breathing chemical fumes, factory dust, soot, or secondhand smoke over a long period of time. COPD can also be caused by a gene change that affects the body's ability to protect the lungs from damage.
What are the symptoms?
The main symptoms of COPD include being short of breath and having a cough that won't go away. You may also cough up mucus. Sometimes your symptoms may get worse over a short time.
How is it diagnosed?
To find out if you have COPD, your doctor will do a physical exam, ask questions about your health, and may do blood tests. Your doctor may do a chest X-ray to look at your lungs and have you do breathing tests to find out how well your lungs work.
How is COPD treated?
COPD may be treated with medicines like bronchodilators to help you breathe easier. Some people also use oxygen therapy to help relieve symptoms. Ask your doctor if pulmonary rehabilitation might be right for you. It includes education, exercise, and support to help people with breathing problems.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
COPD is often caused by smoking. Most people with COPD have smoked for a long time. Over time, breathing tobacco smoke irritates the airways and damages the lungs.
Air pollution also causes COPD. Other things that may lead to COPD include breathing chemical fumes, factory dust, soot, and secondhand smoke over a long period of time.
People who get emphysema at a young age, such as in their 30s or 40s, may have a disorder that runs in families, called alpha-1 antitrypsin deficiency. This is a condition in which your body may not be able to make enough of a protein (alpha-1 antitrypsin) that helps protect the lungs from damage.
Learn more
What Increases Your Risk
Things that put you at risk for COPD include:
- Tobacco smoking.
- Tobacco smoking is the most important risk factor for COPD. The risk for COPD increases with both the amount of tobacco you smoke each day and the number of years you have smoked.
- Breathing in things that can irritate your lungs.
- These things include chemical fumes, factory dust, soot, secondhand smoke, or air pollution over a long period of time.
- Asthma.
- Asthma and COPD are different diseases, even though both of them involve breathing problems. People with asthma may have a greater risk for getting COPD. The reasons for this are not fully understood.
Prevention
You can help prevent COPD by not smoking. If you smoke, quit or cut back as much as you can to prevent COPD from getting worse. Try to avoid things that can irritate your lungs such as chemical fumes, factory dust, soot, and air pollution.
Learn more
Symptoms
The main symptoms are:
- A cough that will not go away.
- Mucus that comes up when you cough.
- Shortness of breath that gets worse with activity.
Sometimes your symptoms may get worse over a short time and stay bad. This is called a COPD exacerbation (say "ig-ZAS-ur-BAY-shun") or flare-up. A flare-up can be dangerous, so it's important to know what to do and take action. Your doctor can help you make a plan to manage flare-ups.
Symptoms of a flare-up include:
- More shortness of breath than usual.
- Coughing more than usual.
- A change in the amount, color, or thickness of mucus.
Symptoms of a COPD flare-up
In a COPD attack or flare-up, your usual symptoms suddenly get worse. You have more shortness of breath and wheezing. You have more coughing, with or without mucus. You may cough up more mucus than usual, and it may be a different color.
What Happens
COPD often gets worse over time. And some people may get lung infections and heart problems. But treatment can help you feel better and prevent symptoms from getting worse quickly. Some treatment may also slow the disease and help you live longer.
Shortness of breath gets worse as COPD gets worse.
- Early in the disease, you may not have much trouble breathing, even when you are active.
- Later in the disease, air doesn't flow as easily in and out of your lungs. You may be short of breath more easily or sooner than you used to when you are active.
- When you've had COPD for many years, you may be short of breath even when you are at rest. Even simple activities may cause bad shortness of breath. For example, you may be short of breath when you do things like get dressed, fix a meal, or eat. People often feel weaker too.
If you smoke, quitting can slow the rate at which breathing gets more difficult. You can't undo the damage to your lungs. But you may be able to postpone or avoid more serious problems with breathing.
Problems from COPD
Health problems that can happen with COPD include:
- More frequent lung infections, such as pneumonia.
- A higher risk of thin or brittle bones (osteoporosis) and broken bones, especially if you use oral corticosteroids often.
- Heart failure or an irregular heartbeat.
- A collapsed lung (pneumothorax). COPD can damage the lung's structure and allow air to leak into the chest cavity.
- Sleep problems.
- Having anxiety or depression.
Learn more
When to Call a Doctor
Call 911 or other emergency services now if:
- Breathing stops.
- Moderate to severe difficulty breathing occurs. This means a person may have trouble talking in full sentences or breathing during activity.
- Severe chest pain occurs, or chest pain is quickly getting worse.
- You cough up large amounts of bright red blood.
Call your doctor immediately or go to the emergency room if you have been diagnosed with COPD and you:
- Cough up a moderate amount of blood (more than a few tablespoons).
- Have shortness of breath or wheezing that is quickly getting worse.
- Start having new chest pain.
- Are coughing more deeply or more often, especially if you notice an increase in mucus (sputum) or a change in the color of the mucus you cough up.
- Have increased swelling in your legs or belly.
- Have a high fever.
- Develop flu-like symptoms.
If your symptoms (cough, mucus, and/or shortness of breath) suddenly get worse and stay worse, you may be having a COPD flare-up, or exacerbation. Quick treatment for a flare-up may help keep you out of the hospital.
Call your doctor soon for an appointment if:
- Your medicine is not working as well as it had been.
- Your symptoms are slowly getting worse, and you have not seen a doctor recently.
- You have a cold and:
- Your fever lasts longer than 2 to 3 days.
- Breathlessness occurs or becomes noticeably worse.
- Your cough gets worse.
- You have not been diagnosed with COPD but are having symptoms. A history of smoking (even in the past) greatly increases the likelihood that symptoms are from COPD.
- You cough up any amount of blood.
- You feel sad, anxious, or hopeless for more than a few days.
Talk to your doctor
If you have been diagnosed with COPD, talk with your doctor at your next regular appointment about:
- Help to stop smoking.
- A yearly flu vaccine.
- The pneumococcal and whooping cough (pertussis) vaccines.
- An exercise program or pulmonary rehabilitation.
- Any updates of your medicines or treatment that you may need.
Exams and Tests
To find out if you have COPD, your doctor may:
- Do a physical exam and listen to your lungs.
- Ask you questions about your past health and whether you smoke or have been exposed to other things that can irritate your lungs.
- Have you do breathing tests, including spirometry, to find out how well your lungs work. These tests measure the amount of air in your lungs and the speed at which air moves in and out.
- Do a chest X-ray to look at your lungs.
- Do a one-time test for alpha-1 antitrypsin (AAT). AAT is a protein your body makes that helps protect the lungs. People who have a low AAT are more likely to get emphysema.
- Do other tests to help rule out other problems that could be causing your symptoms, such as anemia or heart failure.
Your doctor may order other tests, as needed. These may include:
- Arterial blood gas test.
- This test measures how much oxygen, carbon dioxide, and acid is in your blood.
- Oximetry.
- This test measures the oxygen saturation in your blood.
- Electrocardiogram (ECG, EKG) or echocardiogram.
- These tests may find certain heart problems that can cause shortness of breath.
- Diffusing capacity for carbon monoxide (DLCO).
- This test checks how well your lungs can move gas from the air you breathe into your blood. If lungs are damaged from COPD, they may not move gas as well.
- CT scan.
- This gives doctors a detailed picture of the lungs.
Learn more
Treatment Overview
COPD may be treated with medicines and oxygen, along with self-care. Treatment can help you feel better and prevent flare-ups. Some treatments may also slow the disease and help you live longer.
Medicines
Medicines used to treat COPD include:
- Bronchodilators. There are different types of these medicines. They are used to open or relax your airways. They can help you breathe easier and prevent breathing problems.
- Other medicines, such as corticosteroids, may be used to help you feel better and prevent or treat flare-ups.
Oxygen therapy
Oxygen therapy boosts the amount of oxygen in your blood and helps you breathe easier. It can help people with very bad COPD and low oxygen levels live longer.
Self-care
There are things you can do for yourself to help manage your COPD. These include:
- Trying to quit smoking or cutting back as much as you can. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
- Eating healthy.
- Staying as active as possible.
- Learning breathing methods to help you become less short of breath.
- Avoiding colds, infections, and other things that may trigger your symptoms.
- Staying current on vaccines.
Other treatment
- Ask your doctor if pulmonary rehabilitation (rehab) is right for you. Rehab can help relieve your shortness of breath and improve your quality of life. This is a program that uses education, exercise, and support to help people with breathing problems. The programs are designed based on your health needs and your goals.
- You may choose palliative care to help relieve your shortness of breath and improve your quality of life.
- You can plan ahead for what kind of care you want if you become very ill. This is called advance care planning.
- Surgery or certain procedures may be an option for some people. Examples include lung volume reduction and placing an endobronchial valve (EBV).
Treating a COPD flare-up
Treatment of a COPD flare-up, or attack, depends on how bad the flare-up is. Mild flare-ups may be treated by following your doctor's instructions for using a quick-relief (short-acting) inhaler or oral steroid medicines. More severe flare-ups may involve visits to your doctor's office or clinic. Or you may need to be treated in the hospital. Treatments include:
- Quick-relief inhaled bronchodilators. These medicines relax the bronchial tubes and make it easier to breathe.
- Oral steroid medicines. They reduce the swelling in your airways.
- A machine to help you breathe better or to breathe for you. These are called ventilation machines.
- Oxygen, to increase the amount of oxygen in your blood.
Treatment may also include:
- Intravenous (I.V.) fluids to treat dehydration.
- Other bronchodilators.
- Antibiotics. Your doctor may prescribe antibiotics to help treat a bacterial infection.
Learn more
Self-Care
There are many things you can do to help manage COPD. These things may help slow the disease, help you feel better, and help prevent flare-ups.
Quit smoking
If you smoke, try to quit or cut back as much as you can. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
Not smoking is the most important thing you can do to slow down the disease. Quitting also helps relieve your symptoms and reduces flare-ups. It may also help you live longer.
Take your medicines as prescribed
Take your medicines exactly as prescribed. Medicines can help you breathe easier and feel better. Some medicines can help prevent flare-ups and may also help you live longer.
Ask your doctor, pharmacist, or respiratory therapist how to use each of your inhalers correctly. With correct use, the medicine is more likely to get to your lungs.
Try to avoid things that can irritate your lungs
Try to avoid things that could make your symptoms worse. These include secondhand smoke, chemical fumes, factory dust, soot, and air pollution.
Talk to your doctor about ways to protect yourself if you are exposed to substances that irritate your lungs at home or at work.
Find ways to make breathing easier
Here are some ways you can make breathing easier.
- Conserve your energy. You may get more tasks done and feel better if you learn to save energy while doing chores and other activities. For instance, take rest breaks and sit down whenever you can while you fold laundry, cook, and do other household tasks. An occupational or physical therapist can help you find ways to do everyday activities with less effort.
- Learn breathing methods that help you slow down and control your breathing. These methods include pursed lip breathing and belly breathing. Use these methods when you are more short of breath than usual. Practice them often so you can use them correctly when you need to.
- Learn and use ways to clear the mucus in your lungs. These ways include postural drainage and controlled coughing. They can help you save energy and improve your breathing.
Stay as active as you can
Try to do activities and exercises that build muscle strength and help your heart.
Pay attention to your breathing. You are exercising too hard if you can't talk while you exercise. If you get out of breath, wait until your breathing is back to normal before you keep going.
If your doctor has not set you up with a pulmonary rehabilitation program, ask if rehab is right for you. Rehab includes exercise programs, education about your disease and how to manage it, help with diet and other changes, and emotional support.
Eat healthy
Try to eat regular, healthy meals.
Getting enough to eat will help you keep up your strength. If you are losing weight without trying to, ask your doctor or dietitian about ways to make it easier to get the calories you need.
Avoid COVID-19, colds, and the flu
Stay up to date on vaccines. Get a flu vaccine every year. Stay up to date on your COVID-19 vaccines. Get the pneumococcal and whooping cough (pertussis) vaccines. If you have had these vaccines before, ask your doctor if you need another dose. Get the shingles vaccine. Ask your doctor if the RSV (respiratory syncytial virus) vaccine is right for you.
Try other things that can help you avoid lung infections. These include washing your hands often. You may want to wear a mask when you go to public indoor places. Try to avoid sick people.
Watch for changes in your symptoms
If your symptoms get worse over a short time and stay bad, it's called a flare-up. A flare-up can be dangerous, so it's important to know what to do and take action. Your doctor can help you make a plan to manage flare-ups.
Mental health
- Tell your doctor if you feel sad, depressed, or hopeless. Also tell your doctor if you have lost interest in things you usually enjoy or if you have been nervous, worried, or on edge. If needed, medicine and counseling can help.
- Seek connections. Spend time with friends, family, and others. Joining a support group for people with COPD may help.
Stay as healthy as possible
- Educate yourself and your family about COPD and your treatment program. This helps you and your family cope with your lung disease.
- Try to get 7 to 9 hours of sleep each night.
- Try to manage stress. You might try different ways to reduce stress, such as physical activity or deep breathing.
- Take care of your teeth and gums. Get regular dental checkups. This can help you stay healthy.
- Ask for help if your symptoms make it hard for you to do things in the same way you did before. Ask for help from family, friends, neighbors, and others. And try to accept help if it's offered.
Learn more
Surgery
Lung surgery is rarely used to treat COPD. Surgery is never the first treatment choice and is only considered for people who have severe COPD that has not improved with other treatment.
Surgery choices include:
- Lung volume reduction surgery.
This removes part of one or both lungs. It makes room for the rest of the lung to work better. It is used only for some types of severe emphysema.
- Lung transplant.
This surgery replaces a sick lung with a healthy lung from a person who has just died.
- Bullectomy.
This removes the part of the lung that has been damaged by the formation of large, air-filled sacs called bullae. This surgery is rarely done.
Other procedures:
- Bronchoscopic interventions.
These non-surgical techniques collapse (or close off) diseased parts of the lungs to help the remaining parts work better. An example is endobronchial valve therapy.
Learn more
Related Information
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.